Abstract
Introduction:
Bone marrow transplant, both Autograft and Allograft produces profound immune-suppression and breach of mucosal surfaces leading to many opportunistic infections. There is a difference between infection pattern in countries like India compared to western countries. The western literature is more bothered about reactivation of viral and fungal infections, whereas Indian bone marrow transplant physicians are worried about losing patient to refractory gram negative sepsis. In this study, we have tried to decode the pattern of bacterial infections in Indian transplant patients and tried to suggest an antibiotic stewardship for the same.
Materials and methods:
This retrospective study included all bone marrow transplants with Febrile neutropenia done at our hospital from September 2014 to July 2021. A total of 440 patients were included and their pattern of bacterial infections with culture sensitivity and response to antibiotics were noted.
Results:
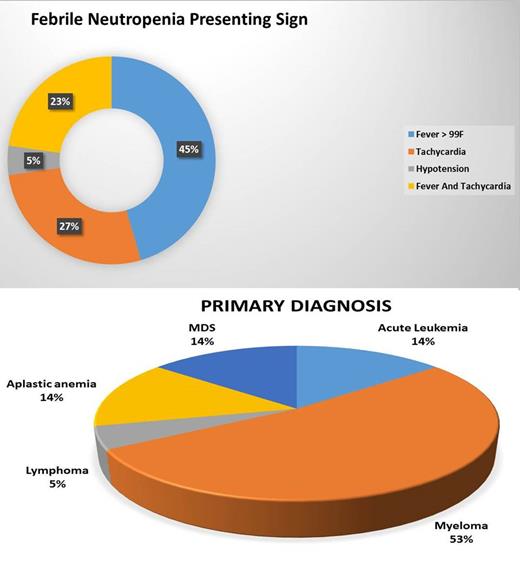
36% of patients we included in the study were aged between 40 to 60 years and the age range was from 2 years to 72 years. 59% were autograft and among Allograft 36% were haplo-identical bone marrow transplant. Nearly half the patients presented with fever above 99.5 F and tachycardia as the presenting sign. The WBC count during first episode febrile neutropenia was less than 100cells/cumm in around 25% patients. Empirical antibiotics post culture samples were initiated within 10 min in 95% of patients. Cefoperazone Sulbactum and Amikacin were started empirically as first line in all.
Culture positivity rate was 22.7% of which 60% were multi-drug resistant gram negative bacilli which were sensitive only to Colistin / Fosfomycin / Tigecycline. This 60% MDR GNB is very high which may be partially due to MDR bugs in normal intestinal flora of patients from this part of the world. The common Gram-negative bacteria are Pseudomonas, Escherichia coli and Klebsiella. This made us to change antibiotic stewardship policy to Colistin / Fosfomycin / Ceftazidime avibactum very early in course in case of second fever / Hypotension or tachycardia. Our transplant related mortality is around 3% in Allograft due to sepsis and 0% in autograft. The rate of gram positive bacteremia is only 2% and this makes us think of avoiding drugs like Teicoplanin / Glycopeptides in first line empirical therapy.
Conclusion:
This seven year study had shown 22.7% culture positivity rate in febrile neutropenia transplant patients of which 60% are multi-drug resistant bacteria which is highly contrary to western literature. The rate of gram positive culture growth is only 2% which is lower than western literature. This study implies the importance of region and center specific antibiotic policy for febrile neutropenia and a generalized policy may not work always.
Reference:-
1. Ghafur A, Devarajan V, Raj R, Easow J, Raja T. Spectrum of bacteremia in posthematopoietic stem cell transplant patients from an Indian center. Indian J Cancer 2016;53:590-1
2. Krüger W,et al. Early infections in patients undergoing bone marrow or blood stem cell transplantation--a 7 year single centre investigation of 409 cases. Bone Marrow Transplant. 1999 Mar;23(6):589-97. doi: 10.1038/sj.bmt.1701614. PMID: 10217190.
No relevant conflicts of interest to declare.